Perspiration
This article about biology may be excessively human-centric. |
| Perspiration | |
|---|---|
| Other names | Sweating, hidrosis, diaphoresis |
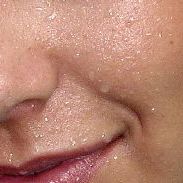 | |
| Droplets of perspiration on the skin | |
| Specialty | Dermatology |
| Symptoms | Body odor |
| Complications | Dehydration |
| Causes | Exercise Fever Heat Hyperthermia Hot flash |
| Prevention | Drinking water |
| Treatment | Antiperspirant |
Perspiration, also known as sweat, is the fluid secreted by sweat glands in the skin of mammals.[1]
Two types of sweat glands can be found in humans: eccrine glands and apocrine glands.[2] The eccrine sweat glands are distributed over much of the body and are responsible for secreting the watery, brackish sweat most often triggered by excessive body temperature. Apocrine sweat glands are restricted to the armpits and a few other areas of the body and produce an odorless, oily, opaque secretion which then gains its characteristic odor from bacterial decomposition.
In humans, sweating is primarily a means of thermoregulation, which is achieved by the water-rich secretion of the eccrine glands. Maximum sweat rates of an adult can be up to 2–4 litres (0.5–1 US gal) per hour or 10–14 litres (2.5–3.5 US gal) per day, but is less in children prior to puberty.[3][4][5] Evaporation of sweat from the skin surface has a cooling effect due to evaporative cooling. Hence, in hot weather, or when the individual's muscles heat up due to exertion, more sweat is produced. Animals with few sweat glands, such as dogs, accomplish similar temperature regulation results by panting, which evaporates water from the moist lining of the oral cavity and pharynx.
Although sweating is found in a wide variety of mammals,[6][7] relatively few (apart from humans, horses, some primates and some bovidae) produce sweat in order to cool down.[8] In horses, such cooling sweat is created by apocrine glands[9] and contains a wetting agent, the protein latherin which transfers from the skin to the surface of their coats.[10]
Definitions
[edit]- The words diaphoresis and hidrosis can both mean either perspiration (in which sense they are synonymous with sweating)[11][12] or excessive perspiration (in which sense they can be either synonymous with hyperhidrosis or differentiable from it only by clinical criteria involved in narrow specialist senses of the words).
- Hypohidrosis is decreased sweating from whatever cause.[13]
- Focal hyperhidrosis is increased or excessive sweating in certain regions such as the underarm, palms, soles, face, or groin.
- Hyperhidrosis is excessive sweating, usually secondary to an underlying condition (in which case it is called secondary hyperhidrosis) and usually involving the body as a whole (in which case it is called generalized hyperhidrosis).[13]
- Hidromeiosis is a reduction in sweating that is due to blockages of sweat glands in humid conditions.[14]
- A substance or medicine that causes perspiration is a sudorific or sudatory.
Signs and symptoms
[edit]Sweat contributes to body odor when it is metabolized by bacteria on the skin. Medications that are used for other treatments and diet also affect odor. Some medical conditions, such as kidney failure and diabetic ketoacidosis, can also affect sweat odor.[citation needed]
Causes
[edit]This section needs additional citations for verification. (March 2016) |

Diaphoresis is a non-specific symptom or sign, which means that it has many possible causes. Some causes of diaphoresis include physical exertion, menopause, fever, ingestion of toxins or irritants, and high environmental temperature. Strong emotions (anger, fear, anxiety) and recall of past trauma can also trigger sweating. This is sometimes referred to as flop sweat.[15]
The vast majority of sweat glands in the body are innervated by sympathetic cholinergic neurons.[16] Sympathetic postganglionic neurons typically secrete norepinephrine and are named sympathetic adrenergic neurons; however, the sympathetic postganglionic neurons that innervate sweat glands secrete acetylcholine and hence are termed sympathetic cholinergic neurons. Sweat glands, piloerector muscles, and some blood vessels are innervated by sympathetic cholinergic neurons.
Pathological sweating and symptoms
[edit]Diaphoresis may be associated with some abnormal conditions, such as hyperthyroidism and shock. If it is accompanied by unexplained weight loss, fever/chills, or by palpitations, shortness of breath, unconsciousness, fatigue, dizziness, muscle pain, nausea, vomiting, diarrhea, and chest discomfort, it suggests serious illness.
Diaphoresis is also seen in an acute myocardial infarction (heart attack), from the increased firing of the sympathetic nervous system, and is frequent in serotonin syndrome, which can result in serious sickness or even death. Diaphoresis can also be caused by many types of infections, often accompanied by high fever and/or chills which can trigger the result of hyperthermia. Most infections can cause some degree of diaphoresis and it is a very common symptom in some serious infections such as malaria and tuberculosis. In addition, pneumothorax can cause diaphoresis with splinting of the chest wall. Neuroleptic malignant syndrome and other malignant diseases (e.g. leukemias) can also cause diaphoresis.[17]
Diabetics relying on insulin shots or oral medications may have low blood sugar (hypoglycemia), which can also cause diaphoresis.
Drugs (including caffeine, morphine, alcohol, antidepressants and certain antipsychotics) may be causes, as well as withdrawal from alcohol, benzodiazepines, nonbenzodiazepines or narcotic painkiller dependencies. Sympathetic nervous system stimulants such as cocaine and amphetamines have also been associated with diaphoresis. Diaphoresis due to ectopic catecholamine is a classic symptom of a pheochromocytoma, a rare tumor of the adrenal gland. Acetylcholinesterase inhibitors (e.g. some insecticides) also cause contraction of sweat gland smooth muscle leading to diaphoresis. Mercury is well known for its use as a diaphoretic, and was widely used in the 19th and early 20th century by physicians to "purge" the body of an illness. However, due to the high toxicity of mercury, secondary symptoms would manifest, which were erroneously attributed to the former disease that was being treated with mercurials.[citation needed]
Infantile acrodynia (childhood mercury poisoning) is characterized by excessive perspiration. A clinician should immediately consider acrodynia in an afebrile child who is sweating profusely.
Some people can develop a sweat allergy.[18][19] The allergy is not due to the sweat itself but instead to an allergy-producing protein secreted by bacteria found on the skin.[19]: 52 Tannic-acid has been found to suppress the allergic response along with showering.[18]
Hyperhidrosis
[edit]Millions of people are affected by hyperhidrosis, but more than half never receive treatment due to embarrassment, lack of awareness, or lack of concern.[20] While it most commonly affects the armpits, feet, and hands, it is possible for someone to experience this condition over their whole body. The face is another common area for hyperhidrosis to be an issue. Sweating uncontrollably is not always expected and may be embarrassing to people with the condition. It can cause both physiological and emotional problems in patients. It is generally inherited.[20] It is not life-threatening, but it is threatening to a person's quality of life.[21] Treatments for hyperhidrosis include antiperspirants, iontophoresis, and surgical removal of sweat glands. In severe cases, botulinum toxin injections or surgical cutting of nerves that stimulate the excessive sweating (endoscopic thoracic sympathectomy) may be an option.[20]
Night sweats
[edit]Night sweats, also known as nocturnal hyperhidrosis, is the occurrence of excessive sweating during sleep. The person may or may not also perspire excessively while awake.
One of the most common causes of night sweats in women over 40 is the hormonal changes related to menopause and perimenopause. This is a very common occurrence during the menopausal transition years.
While night sweats might be relatively harmless, it can also be a sign of a serious underlying disease. It is important to distinguish night sweats due to medical causes from those that occur simply because the sleep environment is too warm, either because the bedroom is unusually hot or because there are too many covers on the bed. Night sweats caused by a medical condition or infection can be described as "severe hot flashes occurring at night that can drench sleepwear and sheets, which are not related to the environment". Some of the underlying medical conditions and infections that cause these severe night sweats can be life-threatening and should promptly be investigated by a medical practitioner.[citation needed]
Mechanism
[edit]
Sweating allows the body to regulate its temperature. Sweating is controlled from a center in the preoptic and anterior regions of the brain's hypothalamus, where thermosensitive neurons are located. The heat-regulatory function of the hypothalamus is also affected by inputs from temperature receptors in the skin. High skin temperature reduces the hypothalamic set point for sweating and increases the gain of the hypothalamic feedback system in response to variations in core temperature. Overall, however, the sweating response to a rise in hypothalamic ('core') temperature is much larger than the response to the same increase in average skin temperature.[citation needed]
Sweating causes a decrease in core temperature through evaporative cooling at the skin surface. As high energy molecules evaporate from the skin, releasing energy absorbed from the body, the skin and superficial vessels decrease in temperature. Cooled venous blood then returns to the body's core and counteracts rising core temperatures.[citation needed]
There are two situations in which the nerves will stimulate the sweat glands, causing perspiration: during physical heat and during emotional stress. In general, emotionally induced sweating is restricted to palms, soles, armpits, and sometimes the forehead, while physical heat-induced sweating occurs throughout the body.[22]
People have an average of two to four million sweat glands, but how much sweat is released by each gland is determined by many factors, including sex, genetics, environmental conditions, age and fitness level. Two of the major contributors to sweat rate are an individual's fitness level and weight. If an individual weighs more, sweat rate is likely to increase because the body must exert more energy to function and there is more body mass to cool down. On the other hand, a fit person will start sweating earlier and more readily. As someone becomes fit, the body becomes more efficient at regulating the body's temperature and sweat glands adapt along with the body's other systems.[23]
Human sweat is not pure water; though it contains no protein, it always contains a small amount (0.2–1%) of solute. When a person moves from a cold climate to a hot climate, adaptive changes occur in the sweating mechanisms of the person. This process is referred to as acclimatization: the maximum rate of sweating increases and its solute composition decreases. The volume of water lost in sweat daily is highly variable, ranging from 100 to 8,000 millilitres per day (0.041 to 3.259 imp fl oz/ks). The solute loss can be as much as 350 mmol/d (or 90 mmol/d acclimatised) of sodium under the most extreme conditions. During average intensity exercise, sweat losses can average up to 2 litres (0.44 imp gal; 0.53 US gal) of water/hour. In a cool climate and in the absence of exercise, sodium loss can be very low (less than 5 mmol/d). Sodium concentration in sweat is 30–65 mmol/L, depending on the degree of acclimatisation.[citation needed]
Horses have a thick, waterproofed, hairy coat that would normally block the rapid translocation of sweat water from the skin to the surface of the hair required for evaporative cooling. To solve this, horses have evolved a detergent-like protein, latherin, that they release at high concentrations in their sweat.[10] Their perspiration unlike humans is created by apocrine glands.[9] This protein, by wetting the horses' coat hairs facilitate water flow for cooling evaporation. The presence of this protein can be seen in the lathering that often occurs on the coats of sweating horses, especially when rubbed.[10] In hot conditions, horses during three hours of moderate-intensity exercise can lose 30 to 35 litres (6.6 to 7.7 imp gal; 7.9 to 9.2 US gal) of water and 100 grams (3.5 oz) of sodium, 198 grams (7.0 oz) of chloride and 45 grams (1.6 oz) of potassium.[9]
Composition
[edit]
Sweat is mostly water. A microfluidic model of the eccrine sweat gland provides details on what solutes partition into sweat, their mechanisms of partitioning, and their fluidic transport to the skin surface.[24] Dissolved in the water are trace amounts of minerals, lactic acid, and urea. Although the mineral content varies, some measured concentrations are: sodium (0.9 gram/litre), potassium (0.2 g/L), calcium (0.015 g/L), and magnesium (0.0013 g/L).[25]
Relative to the plasma and extracellular fluid, the concentration of Na+ ions is much lower in sweat (~40 mM in sweat versus ~150 mM in plasma and extracellular fluid). Initially, within eccrine glands sweat has a high concentration of Na+ ions. In the sweat ducts, the Na+ ions are re-absorbed into tissue by epithelial sodium channels (ENaC) that are located on the apical membrane of epithelial cells that form the duct (see Fig. 9 of the reference).[2]
Many other trace elements are also excreted in sweat, again an indication of their concentration is (although measurements can vary fifteenfold) zinc (0.4 milligrams/litre), copper (0.3–0.8 mg/L), iron (1 mg/L), chromium (0.1 mg/L), nickel (0.05 mg/L), and lead (0.05 mg/L).[26][27] Probably many other less-abundant trace minerals leave the body through sweating with correspondingly lower concentrations. Some exogenous organic compounds make their way into sweat as exemplified by an unidentified odiferous "maple syrup" scented compound in several of the species in the mushroom genus Lactarius.[28] In humans, sweat is hypoosmotic relative to plasma[29] (i.e. less concentrated). Sweat is found at moderately acidic to neutral pH levels, typically between 4.5 and 7.0.[30]
Sweat contains many glycoproteins.[31]
Other functions
[edit]Antimicrobial
[edit]Sweat may serve an antimicrobial function, like that of earwax or other secretory fluids (e.g., tears, saliva, and milk).[clarification needed] It does this through a combination of glycoproteins that either bind directly to, or prevent the binding of microbes to, the skin and seem to form part of the innate immune system.[31]
In 2001, researchers at Eberhard-Karls University in Tübingen, Germany, isolated a large protein called dermcidin from skin. This protein, which could be cleaved into other antimicrobial peptides, was shown to be effective at killing some species of bacteria and fungi that affect humans, including Escherichia coli, Enterococcus faecalis, Staphylococcus aureus, and Candida albicans. It was active at high salt concentrations and in the acidity range of human sweat, where it was present at concentrations of 1–10 mg/ml.[32][33]
Society and culture
[edit]Artificial perspiration
[edit]Artificial skin capable of sweating similar to natural sweat rates and with the surface texture and wetting properties of regular skin has been developed for research purposes.[34][35] Artificial perspiration is also available for in-vitro testing, and contains 19 amino acids and the most abundant minerals and metabolites in sweat.[citation needed]
Diagnostics
[edit]There is interest in its use in wearable technology. Sweat can be sampled and sensed non-invasively and continuously using electronic tattoos, bands, or patches.[36] However, sweat as a diagnostic fluid presents numerous challenges as well, such as very small sample volumes and filtration (dilution) of larger-sized hydrophilic analytes. Currently the only major commercial application for sweat diagnostics is for infant cystic fibrosis testing based on sweat chloride concentrations.[citation needed]
See also
[edit]References
[edit]- ^ Mosher, H. H. (1 February 1933). "Simultaneous Study of Constituents of Urine and Perspiration". Journal of Biological Chemistry. 99 (3): 781–790. doi:10.1016/S0021-9258(18)76026-2. S2CID 43499897.
- ^ a b Hanukoglu I, Boggula VR, Vaknine H, Sharma S, Kleyman T, Hanukoglu A (January 2017). "Expression of epithelial sodium channel (ENaC) and CFTR in the human epidermis and epidermal appendages". Histochemistry and Cell Biology. 147 (6): 733–748. doi:10.1007/s00418-016-1535-3. PMID 28130590. S2CID 8504408.
- ^ Jessen, C. (2000). Temperature Regulation in Humans and Other Mammals. Berlin: Springer. ISBN 978-3-540-41234-2.
- ^ Mack, G. W.; Nadel, E. R. (1996). "Body fluid balance during heat stress in humans". In Fregly, M. J.; Blatteis, C. M. (eds.). Handbook of Physiology. Section 4: Environmental Physiology. New York: Oxford University Press. pp. 187–214. ISBN 978-0-19-507492-5.
- ^ Sawka, M. L.; Wenger, C. B.; Pandolf, K. B. (1996). "Thermoregulatory responses to acute exercise-heat stress and heat acclimation". In Fregly, M. J.; Blatteis, C. M. (eds.). Handbook of Physiology. Section 4: Environmental Physiology. New York: Oxford University Press. ISBN 978-0-19-507492-5.
- ^ Goglia, G (January 1953). "Italian: Cavia cobaya, Sus scrofa, Equus caballus" [Further research on the branched sweat glands in some mammals]. Bollettino della Società Italiana di Biologia Sperimentale (in Italian). 29 (1): 58–60. PMID 13066656.
- ^ Robertshaw D, Taylor CR (November 1969). "Sweat gland function of the donkey (Equus asinus)". The Journal of Physiology. 205 (1): 79–89. doi:10.1113/jphysiol.1969.sp008952. PMC 1348626. PMID 5347721.
- ^ Jenkinson, D. McEwan (April 1973). "Comparative Physiology of Sweating". British Journal of Dermatology. 88 (4): 397–406. doi:10.1111/j.1365-2133.1973.tb07573.x. PMID 4582049. S2CID 35727313.
- ^ a b c McCutcheon, L. Jill; Geor, Raymond J. (1998). "Sweating: Fluid and Ion Losses and Replacement". Veterinary Clinics of North America: Equine Practice. 14 (1): 75–95. doi:10.1016/s0749-0739(17)30213-4. ISSN 0749-0739. PMID 9561689.
- ^ a b c McDonald RE, Fleming RI, Beeley JG, et al. (2009). Koutsopoulos S (ed.). "Latherin: A Surfactant Protein of Horse Sweat and Saliva". PLOS ONE. 4 (5): e5726. Bibcode:2009PLoSO...4.5726M. doi:10.1371/journal.pone.0005726. PMC 2684629. PMID 19478940.
- ^ Elsevier, Dorland's Illustrated Medical Dictionary, Elsevier.
- ^ Wolters Kluwer, Stedman's Medical Dictionary, Wolters Kluwer.
- ^ a b "Academy of Hyperhidrosis". Allaboutsweat.com. Archived from the original on 2018-12-27. Retrieved 2014-04-05.
- ^ Parsons K (2009). "Maintaining health, comfort and productivity in heat waves". Glob Health Action. 2: 2057. doi:10.3402/gha.v2i0.2057. PMC 2799322. PMID 20052377.
- ^ "Beyond shyness and stage fright: Social anxiety disorder". Harvard Mental Health Letter. 4 April 2010. Retrieved December 8, 2012.
- ^ Boron, Walter F., and Emile L. Boulpaep. "Sweating." Medical Physiology. Updated 2nd ed. Philadelphia: Elsevier, 2012. 1260–264. Print.
- ^ Neuroleptic Malignant Syndrome~clinical at eMedicine
- ^ a b Hiragun, Takaaki; Hiragun, Makiko; Ishii, Kaori; Kan, Takanobu; Hide, Michihiro (July 2017). "Sweat allergy: Extrinsic or intrinsic?". Journal of Dermatological Science. 87 (1): 3–9. doi:10.1016/j.jdermsci.2017.03.002. PMID 28416076.
- ^ a b Yokozeki, Hiroo; Murota, Hiroyuki; Katayama, Ichrio (1 September 2016). "Sweat Allergy". Perspiration Research. Current Problems in Dermatology. Vol. 51. pp. 101–108. doi:10.1159/000446788. ISBN 978-3-318-05904-5. LCCN 2016030383. OCLC 958455309. OL 40308286M. PMID 27584969. Retrieved 13 January 2024 – via Google Books.
- ^ a b c "Hyperhidrosis". MedlinePlus, US National Library of Medicine. 7 June 2023. Retrieved 17 January 2024.
- ^ Kamudoni, P.; Mueller, B.; Halford, J.; Schouveller, A.; Stacey, B.; Salek, M.S. (8 June 2017). "The impact of hyperhidrosis on patients' daily life and quality of life: a qualitative investigation". Health and Quality of Life Outcomes. 15 (1): 121. doi:10.1186/s12955-017-0693-x. ISSN 1477-7525. PMC 5465471. PMID 28595584.
- ^ Kameia, Tomoya; Tsudab, Takao; Kitagawab, Shinya; Naitoha, Ken; Nakashimaa, Koji; Ohhashi, Toshio (5 June 1998). "Physical stimuli and emotional stress-induced sweat secretions in the human palm and forehead". Analytica Chimica Acta. 365 (1–3): 319–326. Bibcode:1998AcAC..365..319K. doi:10.1016/S0003-2670(97)00642-9. eISSN 1873-4324. ISSN 0003-2670. OCLC 01716731.
- ^ Hansen, Julieann (22 May 2013). "The Science of Sweat". American College of Sports Medicine. Archived from the original on 21 September 2013. Retrieved 13 January 2023.
- ^ Sonner, Z.; Wilder, E.; Heikenfeld, J.; Kasting, G.; Beyette, F.; Swaile, D.; Sherman, F.; Joyce, J.; Hagen, J. (2015-05-01). "The microfluidics of the eccrine sweat gland, including biomarker partitioning, transport, and biosensing implications". Biomicrofluidics. 9 (3): 031301. doi:10.1063/1.4921039. ISSN 1932-1058. PMC 4433483. PMID 26045728.
- ^ Montain, S. J.; Cheuvront, S. N.; Lukaski, H. C. (2007). "Sweat mineral-element responses during 7 h of exercise-heat stress". International Journal of Sport Nutrition and Exercise Metabolism. 17 (6): 574–582. doi:10.1123/ijsnem.17.6.574. PMID 18156662. S2CID 3030692.
- ^ Cohn JR, Emmett EA (1978). "The excretion of traces of metals in human sweat". Annals of Clinical and Laboratory Science. 8 (4): 270–5. PMID 686643.
- ^ Saraymen, Recep; Kılıç, Eser; Yazar, Süleyman (2004). "Sweat Copper, Zinc, Iron, Magnesium and Chromium Levels in National Wrestler". İnönü Üniversitesi Tıp Fakültesi Dergisi. 11 (1): 7–10. Archived from the original on 2011-08-20.
- ^ Aurora, David "Lactarius fragilis" Mushrooms Demystified 1986 Ten Speed Press, Berkeley California
- ^ Constanzo, Linda S. BRS Physiology (6th ed.). p. 151.
- ^ Bandodkar AJ, Hung VW, Jia W, Ramirez GV, Windmiller JR, Martinez AG, Ramirez J, Chan G, Kagan K, Wang J (2013). "Tattoo-based potentiometric ion-selective sensors for epidermal pH monitoring". Analyst. 138 (1): 123–8. Bibcode:2013Ana...138..123B. doi:10.1039/c2an36422k. PMID 23113321.
- ^ a b Robyn A Peterson; Audrey Gueniche; Ségolène Adam de Beaumais; Lionel Breton; Maria Dalko-Csiba; Nicolle H Packer (17 November 2015). "Sweating the small stuff: Glycoproteins in human sweat and their unexplored potential for microbial adhesion". Glycobiology. 26 (3): 218–229. doi:10.1093/glycob/cwv102. PMID 26582610.
- ^ Josefson, Deborah (2001-11-24). "Bacteria killer found in sweat". British Medical Journal. 323 (7323): 1206. doi:10.1136/bmj.323.7323.1206c. ISSN 0959-8138. PMC 1173041.
- ^ "DCD dermcidin [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2022-12-04.
- ^ Hou, Linlin; Hagen, Joshua; Wang, Xiao; Papautsky, Ian; Naik, Rajesh; Kelley-Loughnane, Nancy; Heikenfeld, Jason (2013-04-23). "Artificial microfluidic skin for in vitro perspiration simulation and testing". Lab on a Chip. 13 (10): 1868–1875. doi:10.1039/C3LC41231H. PMID 23576120.
- ^ Jain, Vaibhav; Ochoa, Manuel; Jiang, Hongjie; Rahimi, Rahim; Ziaie, Babak (2019-06-17). "A mass-customizable dermal patch with discrete colorimetric indicators for personalized sweat rate quantification". Microsystems & Nanoengineering. 5 (1): 29. Bibcode:2019MicNa...5...29J. doi:10.1038/s41378-019-0067-0. ISSN 2055-7434. PMC 6572848. PMID 31240108.
- ^ Heikenfeld, Jason (2016). "Non-invasive Analyte Access and Sensing through Eccrine Sweat: Challenges and Outlook circa 2016". Electroanalysis. 28 (6): 1242–1249. doi:10.1002/elan.201600018.
Further reading
[edit]- Ferner S, Koszmagk R, Lehmann A, Heilmann W (1990). "[Reference values of Na(+) and Cl(-) concentrations in adult sweat]". Zeitschrift für Erkrankungen der Atmungsorgane (in German). 175 (2): 70–5. PMID 2264363.
- Nadel ER, Bullard RW, Stolwijk JA (July 1971). "Importance of skin temperature in the regulation of sweating". Journal of Applied Physiology. 31 (1): 80–7. doi:10.1152/jappl.1971.31.1.80. PMID 5556967.
- Sato K, Kang WH, Saga K, Sato KT (April 1989). "Biology of sweat glands and their disorders. I. Normal sweat gland function". Journal of the American Academy of Dermatology. 20 (4): 537–63. doi:10.1016/S0190-9622(89)70063-3. PMID 2654204.
External links
[edit] Media related to Perspiration at Wikimedia Commons
Media related to Perspiration at Wikimedia Commons
